Technical Diploma in Antimicrobial Resistance
Description
The Technical Diploma in Antimicrobial Resistance (AMR) provides a structured six-module learning journey that builds participants’ knowledge and skills in addressing AMR from clinical, laboratory, and public health perspectives.
Designed for professionals involved in combating AMR and promoting the rational use of antimicrobials, the program targets medical doctors, pharmacists, microbiologists, infection control practitioners, veterinarians, One Health specialists, and policy or program managers engaged in national AMR action plans, surveillance, and pharmaceutical regulation.
The content covers the classification, detection, and mechanisms of AMR; laboratory identification and susceptibility testing; and the principles of antimicrobial stewardship, including rational prescribing, treatment guidelines, and program design. Advanced modules address AMR surveillance systems, the One Health approach, and multidrug resistance in diseases such as tuberculosis, HIV, and malaria. The final modules focus on applied stewardship practices, integrating rapid diagnostics, infection control measures, and benchmarking techniques to evaluate program performance.
Objectives
Upon completion of the program, participants will be able to:
- Discuss the current debate and thinking surrounding antimicrobial resistance in modern public health.
- Implement and promote advanced antimicrobial stewardship approaches.
- Detect and manage antimicrobial resistance.
- Effectively and efficiently maintain and improve the performance and the outcomes of the antimicrobial resistance stewardship program.
- Combat antimicrobial resistance through effective and efficient HIV, TB, and malaria control programs.
Modality
This Technical Diploma is delivered through a fully self-paced online modality, allowing participants to access all learning materials and activities at their convenience. The program includes interactive content, pre- and post-tests to support knowledge acquisition. Participants can learn at their own pace and revisit modules as needed throughout the course duration.
Target Audience
Designed for healthcare professionals including physicians, pharmacists, nurses, laboratory specialists, veterinarians, and public health practitioners involved in AMR prevention and control.
It is also suitable for researchers, academics, policymakers, and professionals in the pharmaceutical and environmental health sectors.
Certification
Upon successful completion, participants will receive a Technical Diploma in Antimicrobial Resistance issued by the International Academy of Public Health (IAPH).
The program is accredited by the Agency for Public Health Education Accreditation (APHEA).
Admission Requirements
To enroll in this technical diploma, applicants should:
- Hold a bachelor’s degree in medicine, pharmacy, nursing, medical laboratory sciences, veterinary medicine, or a related health or life science field.
- Have professional experience or interest in infectious diseases, microbiology, pharmacology, or public health (preferred but not required).
- Be proficient in English to understand course materials and complete assessments.
- Have access to a computer and reliable internet connection to complete the online learning modules.
Module 1: Antimicrobial Resistance-Level 1
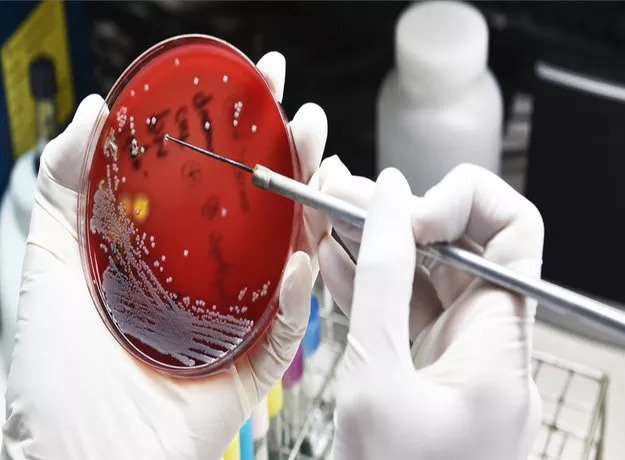
It is important to recognize that laboratory work and clinical experience must be closely integrated; thus, laboratory-associated clinical duties are an essential component of the training program.
This course aims to provide candidates with a theoretical foundation as well as the practical, technical, clinical, and managerial skills required for health care professionals to detect and manage antimicrobial resistance.
Learning Outcomes
By the end of this module, the participant will be able to:
- Describe the basic classification/nomenclature system(s) of microorganisms
- List and compare common methods for isolation, identification and antimicrobial susceptibility testing of microorganisms
- State the basic mechanisms of antimicrobial resistance
- List those pathogenic microorganisms that currently present major treatment challenges due to antimicrobial resistance
- Describe strategies to identify problematic pathogens in a given institution and propose actions to address those challenges to patient care
- List guidelines for assembly of institutional antibiograms and describe potential pitfalls in interpretation of these reports
- Describe and list procedures utilizing antibiogram information to identify and track resistance problems, make appropriate antimicrobial formulary decisions, and to prepare optimal clinical pathways at a given institution
Module Outline
- Pathogenic Microorganisms
- Identification of Microorganism
- Antimicrobial Mode of Action
- Pathogen Isolation and Antimicrobial Sensitivity
- VITEK and PCR Tests
- Antimicrobial and Susceptibility Tests
- Disc Diffusion Method
Module 2: Antimicrobial stewardship-Level 1

Antimicrobial resistance is driven by the overuse of antimicrobials and inappropriate prescribing. The increase in resistance is making antimicrobial agents less effective and contributing to infections that are hard to treat. Antimicrobial stewardship initiatives aim to improve the prescribing of all agents, whether they target bacterial, viral, fungal, mycobacterium, or protozoal infections. Educating the public and healthcare professionals in the prudent use of antimicrobials as part of an antimicrobial stewardship program is of paramount importance to preserve these crucial treatments and to help control resistance. Therefore imperative that the candidate be equipped with knowledge and skills on Antimicrobial stewardship.
Learning Outcomes
By the end of this module, the participant will be able to:
- Demonstrate understanding of the Essential Medicines List (EML) concept, how EML is developed, explaining its role in promoting rational use of medicines, including antimicrobials.
- Explain the importance of Standard Treatment Guidelines and demonstrate the method of developing them, explaining their role in promoting rational use of medicines, including antimicrobials.
- Demonstrate understanding of the Pharmacy & Therapeutics Committees (PTCs) at hospitals and explain their vital role in the rational use of antimicrobials.
- Explain the concept of Hospital formularies and the selection criteria for inclusion of medicines in the hospital formulary depending on different types of health facilities.
- Illustrate the importance of using international nonproprietary names (INN) or generic names in the EML, STG, and hospital formulary
Module Outline
- Basics of Antimicrobial Drugs
- Mechanisms of Antimicrobial Drugs
- Spectrum of Antimicrobial Activity
- Pharmacodynamics of Antimicrobial
- Introduction to Antimicrobial Stewardship
- Introduction to Antibiograms
- Rational Use of Antimicrobial Agents
- Guidelines to Effective Antimicrobial Treatment
Module 3: Antimicrobial Resistance-Level 2

AMR surveillance is the cornerstone for assessing the burden of AMR and for providing the necessary information for action in support of local, national, and global strategies. One of the five strategic objectives of the global antimicrobial resistance action plan that has been adopted by the sixty-eight World Health Assembly is to strengthen the evidence base through enhanced global surveillance and research.
The goal of this module is to equip the candidate with knowledge and skills that enable them to collect, analyze, and share the data on AMR at a global level, to inform decision-making, drive local, national, and regional action, and provide the evidence base for action and advocacy.
Learning Outcomes
By the end of this module, the participant will be able to:
- Work with antimicrobial and diagnostic stewardship multidisciplinary teams
- Practice the international standard for laboratory practice
- Conduct monitoring, evaluation, and development of AMR Surveillance
- Design AMR surveillance system
Module Outline
- International Standards for Laboratory Practice
- Bio-Safety in Laboratory
- Hazardous Pathogens
- Standard Precautions in Laboratory
- Introduction to Antimicrobial Surveillance
- Sterilization and Disinfection
- Technical Components of AMR Surveillance
- Threats of Antibiotic-Resistant Bacteria Outbreak
- Role of the Lab in Antimicrobial Surveillance
- Antimicrobial Consumption Monitoring
Module 4: Antimicrobial Stewardship-Level 2

This module addresses issues of antimicrobial resistance and related genes through an interdisciplinary "One Health" approach, integrating human, animal, and environmental health. It examines the global use and misuse of antimicrobials and their profound impact on the health of humans, animals, and the environment. The goal of this module is to equip candidates with the knowledge, skills, and abilities essential for implementing and promoting Antimicrobial Stewardship.
Learning Outcomes
By the end of this module, the participant will be able to:
- Compare and analyze diverse viewpoints on controversial issues related to sources of ARGs/ARBs in relationship to humans, animals, and the environment (i.e. One Health)
- List and compare methods for prospectively measuring antimicrobial use in an organized healthcare setting
- Prepare and defend a proposal that cost-justifies the funding of a stewardship program
- Document stewardship interventions and assess their effects
- Provide in-service training on a stewardship program to other healthcare providers
Module Outline
- Emergence of Antimicrobial Resistance in Bacteria
- Relevance of Animal Production in the Emergence of Antimicrobial Resistance
- Mechanism of Spread of AMR
- Integrating Rapid Diagnostics into Antimicrobial Stewardship
- Clinical Decision Support Software Session
- Designing Stewardship Interventions
- One Health Approach in Developing NAP-AMR
- Approach to Multisectoral Systems
- Core Components of NAP-AMR
- Antibiotics Policy and Guideline
- Evidence-Based Good Prescription and Dispension
- Chain of Infection
- Best Hygiene Practices
- Epidemiology of Health Care Acquired Infections
- Management of Infection Prevention and Control Programs
- AMR Awareness and Educational Campaign
Module 5: Multidrug Resistance
Resistance to tuberculosis (TB) drugs is a formidable obstacle to effective TB care and prevention globally. Multidrug-resistant TB (MDR-TB) is multifactorial and fueled by improper treatment of patients, poor management of the supply and quality of drugs, and airborne transmission of bacteria in public places. Case management becomes difficult and the challenge is compounded by catastrophic economic and social costs that patients incur while seeking help and spending on treatments.
Learning Outcomes
By the end of this module, the participant will be able to:
- Apply an interdisciplinary epidemiology approach to study TB, HIV, and malaria drug-resistant
- Identify factors that influence HIV, TB, and malaria drug resistance
- Apply strategies for minimizing the development of drug resistance
- Document stewardship interventions and assess their effects
- Apply strategies for responding to the detection of moderate to high levels of drug-resistant HIV, TB, and malaria
Module Outline
- HIV Drug Resistance
- The HIVDR Laboratory Network
- Laboratory Diagnosis of HIVDR
- Control of HIVDR
- Epidemiology of TBDR
- Lab Network for Management of TBMDR
- Rapid Diagnosis of TBDR
- Xpert MTB/RIF
- Multidrug-Resistant Tuberculosis (MDR-TB) Control Strategies
- Challenges to Programmatic Management of Drug-Resistant TB
- Malaria Drug Resistance
- Therapeutic Efficacy Studies
Module 6: Antimicrobial Stewardship-Level 3
This module addresses issues of antimicrobial resistance and genes through an interdisciplinary ''One Health'' approach that integrates human, animal, and environmental health. It explores how global use and abuse of antimicrobials have profound consequences on the health of humans, animals, and the environment. The goal of this module is to provide the candidates with knowledge, skills, and abilities that are critical to implement and promote Antimicrobial Stewardship.
Learning Outcomes
By the end of this module, the participant will be able to:
- Apply advances in antimicrobial stewardship
- Apply advances in antimicrobial therapeutics, including new agents, new vaccines, and pharmacodynamics principles to patient care at the patient and system levels
- Apply epidemiologic and infection control and susceptibility surveillance methods, including the use of electronic data capture software.
- Propose methods for assessing quality improvement through local, national, and international benchmarking techniques
Module Outline
- Advanced Pharmacokinetics/Pharmodynamics
- Indicators to Measure Antimicrobial Prescription
- Global Antimicrobial Resistance Surveillance System
- AMR Data Collection and Reporting
- ASP Costs and Benefits
- Financial Metrics of ASP
- Benchmarking ASPs
Diploma Features:



